Clinical trials are conducted to create evidence. Companies, researchers, physicians, etc. take data from clinical trials and publish it via research papers. Professional societies then create clinical treatment guidelines based off of the publications.
To better understand what's coming down the pipeline and what trials will be influencing future treatment guidelines, I took a look at all RA clinical trials on ClinicalTrials.gov. I narrowed the search down to look at RA studies to be completed between 2015 to 2030.
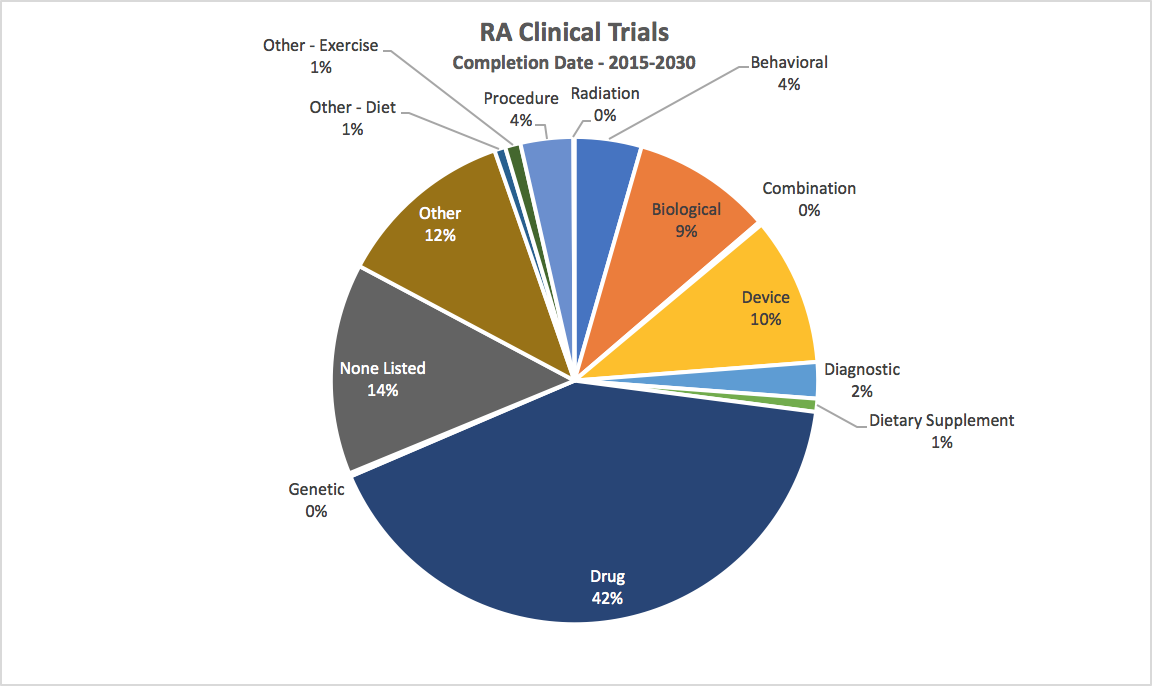
We see a disproportionate number, >50%, of clinical studies focused on drugs and biologics. And, almost 60% if we include devices. A modest 7% of clinical trials are looking at lifestyle impacts, such as exercise and diet.
Why is this? Well, funding. Large pharma players have the capital available to invest in therapies and support large scale clinical trials to influence professional societies, standard of care guidelines, and further product development. Pharma companies get reimbursed fairly well (as we saw in Kawatkar's analysis) for producing "improved outcomes" defined by ACR (as we saw in the ACR '21 Guidelines). Now, this isn't a bad thing. We need innovative, life-saving therapies.
Should these therapies be used as the first line defense? Most would say 'yes' given the research showing they improve "quality of life" and stunt disease progression...well, I hesitantly type that. Do they really improve quality of life given how severe the side effects are? Are they truly slowing progression of the disease?
Are drugs the only way to slow disease progression? We won't know until we study other interventions, therapies, tools, and ways of treating... of healing...

